Yearly Archives: 2015
By David F. Box, M.D.
Shingles is a common disease caused by the chickenpox virus. In the past, primary chickenpox typically occurred during the childhood years. The chickenpox vaccine was developed in 1995 and has been routinely administered to children in developed countries for many years. So, it is currently rare for a healthy child to develop chickenpox after receiving the vaccine. However, as the immunity to chickenpox declines over time, individuals grow susceptible to a secondary infection, which we call shingles. Most commonly, the infection manifests itself as a painful rash occurring on one side of the trunk of the body. The second most common location is on one side of the face and scalp.
If the rash occurs in that second location, it can attack the eye directly, causing permanent visual damage and chronic eye pain. In many cases, the risk of this can be decreased by prompt treatment. At the Indiana Eye Clinic, all of our doctors are thoroughly trained in the emergency management of shingles involving the eye structures. We work closely with your primary care physician to optimize your treatment and minimize the risks of chronic complications.
Prior to the development of the chickenpox vaccine, the lifetime risk of developing shingles was between 10-20 percent in individuals who had suffered from chickenpox earlier in life. Most experts believe that the immunity to chickenpox resulting from the childhood vaccine is not as long-lasting as the immunity from an actual case of chickenpox. Therefore, the incidence of shingles is expected to increase in the future among individuals who were born after the early ’90s. In addition, it is expected that shingles in this group of patients may occur at a younger average age than their predecessors. Not all experts agree on this subject but the shingles vaccine is expected to be recommended for these individuals by the time they reach the age of 50.
If you were born before 1990, you still are faced with a 10-20 percent risk of contracting shingles. Usually the disease would appear after age 60 in your group. Ophthalmologists commonly see patients over age 60 who are suffering from shingles occurring on the face and scalp. In most patients, the disease is self-limiting and resolves without long-term complications in 2-3 weeks. Unfortunately there is a small group of shingles patients who suffer long-term complications of this disease.
The best option for this disease is prevention. The shingles vaccine (Zostavax) has been shown to greatly decrease the risk of shingles. The vaccine is approved by the Food and Drug Administration for adults 50 and older. It is currently recommended for adults 60 and older with normal immune systems and no known allergies to the components of the vaccine.
JOB SUMMARY:
This individual is responsible for performing an extensive number of data collection functions, as delegated by the physician, to allow for proper professional diagnosis of patients’ conditions.
EDUCATION AND EXPERIENCE:
- High school diploma; some college preferred.
- Two to five years experience as an ophthalmic assistant or optician.
- Valid CPR certification preferred.
ESSENTIAL SKILLS AND ABILITIES:
- Demonstrated, advanced comprehension of the ophthalmic assistant skills as outlined by the Joint Commission on Allied Health Personnel in Ophthalmology (JCAHPO).
- Basic understanding of optics and refractometry.
- Strong communication and interpersonal skills.
- Empathetic personality with concern for patients’ needs.
- Strong organization with attention to detail.
- Ability to work as a team member.
- Demonstrated comprehension of the principles of optics, refraction, and contact lenses.
- Demonstrated ability to perform comprehensive work ups on three patients per hour.
- Demonstrated computer literacy.
RESPONSIBILITIES:
- Communication and Patient Care
- Acquaints all new patients with office procedures to which they will be exposed.
- Informs patients of the purpose of all tests personally performed, and how the patient will be affected during the tests.
- Obtains patient history to include chief complaint, history of present illness, past history (ocular and general), family history (ocular and general), and history of allergies and medications.
- Performs accurate and consistent documentation and measurement tasks to include:
- Visual acuity
- Manual lensometry
- Confrontational visual fields
- Stereo testing
- Evaluation of motility
- Pupillary function tests
- Color plates
- Applanation tonometry
- Refractometry
- Angle assessment
- Dilation of pupils
- Contact lens evaluations
- Visual field testing
- Optic nerve scanning (i.e. OCT, HRT)
- Pachymetry
- Corneal topography
- Other tasks specific to the physician’s needs as a result of new technologies
- Provides back-up to the ophthalmic photographer regarding fundus, exterior and anterior segment photographs.
- Performs duties consistent with ophthalmic writer/scribe.
- Assists physician with laser procedures.
- Assists physician with minor surgery, maintaining practice standards of sterile technique and infection control.
- Triage
- Determines which patient should be taken next from the waiting room to have testing initiated.
- Escorts all patients from the waiting room for data collection.
- Advises patients as to who will see them following testing and makes patients comfortable during wait.
- Maintains a smooth flow of patients to the physician, altering the test sequence as required.
- Provides telephone support regarding ocular emergencies, prescription refills, and patient care questions.
- Communicates with reception to facilitate proper patient flow.
- Instrument Maintenance
- Troubleshoots instruments as necessary.
- Replaces bulbs.
- Checks connections.
- Performs archiving functions according to manufacturer recommendations.
- Reports continued difficulty to Clinical Director.
- Administrative
- Seeks advice from more senior staff as necessary, never performing beyond capabilities.
- Maintains cleanliness in exam and procedure rooms.
- Maintains back up levels of stock in exam and procedure rooms.
- Performs other duties as required.
By Dr. Michael L. Hopen, Ophthalmologist
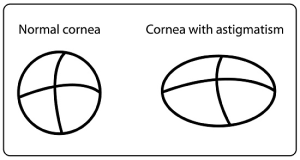
Astigmatism is an optical condition in which light rays from an object do not focus to a single point on the retina because of variations in the curvature of the cornea. Astigmatism can cause blurring and distortion of the vision.
The cornea without astigmatism is a smooth sphere and has the shape and curvature of a basketball. The cornea with astigmatism has a more oblong shaped like that of a football.
We now have many options to treat astigmatism. Many people are satisfied having their astigmatism corrected with glasses. Others prefer specialized contact lenses to correct a certain degree of their astigmatism.
Surgical options for astigmatism management include laser vision correction (e.g., photo refractive keratectomy or PRK), astigmatic keratotomy — during which relaxing incisions are placed in the cornea — and lens-based surgery (cataract surgery).
Neutralizing the astigmatism caused from the cornea with an intraocular lens during cataract surgery is a very effective way to improve the optical system. At the Indiana Eye Clinic, we are able to address a wide range of regular astigmatism with toric intraocular lenses. An added advantage of having surgery at the Indiana Eye Clinic includes our ability to utilize the newest technology during the surgical procedure (such as ORA wavefront) in order to ensure that the toric lens is placed in the optimal position.
Please feel free to ask your Optometrist or Ophthalmologist about your astigmatism correcting options during your next visit!
Sources:
American Academy of Ophthalmology BCSC – Clinical Optics
https://nei.nih.gov/health/errors/astigmatism
http://home2.btconnect.com/alanmilleroptom/Images/Clocks.png
By Carissa M. Barina, M.D., Ophthalmologist
If you spend time in front of a computer, you’re probably familiar with the feeling of having eyes that are tired after long hours staring at a screen. You strain to see well and your head may even hurt. With the surging popularity of smaller devices with visual displays – smartphones, e-readers, tablets, etc. – it has become a more widespread problem.
This has come to be known as Computer Vision Syndrome or Digital Eye Strain. The Vision Council estimates that 70% of U.S. adults experience it in some form.
The reason for this condition is that when you are looking at a computer screen, your eyes must continuously focus, move back and forth, and align with what you are seeing. They must accommodate to changing images on the screen in order to form a clear picture for the brain to interpret.
All of these functions require a great deal of effort by the eye muscles. Doing it for a prolonged amount of time can cause fatigue, blurred vision, double vision, eye irritation and headaches.
In addition, intently focusing on computer activities causes your eyes to blink less frequently – about one-third of their normal blink rate. This contributes to evaporative tear loss, which causes dry, red eyes and blurred vision.
The good news is that there’s no evidence that computer vision syndrome causes long-term damage to the eyes. But it can certainly be a nuisance that negatively impacts your work productivity or enjoyment of computer-assisted tasks.
Fortunately, there are steps you can take to help prevent and improve computer vision symptoms:
- Lighting. Limit excessively bright sunlight or harsh interior lighting at your workstation.
- Glare. Reduce reflections on the computer screen — adjust overhead lights, window shades, etc. – or install a glare filter over the monitor.
- Computer settings and position. Adjust the brightness so that it is approximately the same as the ambient light at your workstation. Adjust contrast and font size on the computer until you find the best settings for your comfort. Find the optimal position for your computer monitor so it is slightly below eye level, about 20 to 28 inches away from the face. Use a monitor with a diagonal screen size of at least 19 inches set at the highest resolution.
- 20/20/20 rule: Look away from the screen every 20 minutes or so. Either gaze out the window or scan the room and focus on a distant object about 20 feet away for about 20 seconds. This will relax the eye muscles.
- Blink more often. Every 10 minutes or so, blink 10 times slowly. This limits dry eye and ocular discomfort and maintains visual clarity. If eye dryness/irritation is especially bad, artificial tears may be necessary to replenish moisture to the ocular surface.
- Routine eye exams. Visit your eye doctor regularly for an exam to ensure your prescriptions are adequate. Your doctor will help determine if you need special computer glasses. These may contain a single or bifocal lens, or tinted lens material, which could help increase contrast perception and filter out glare and reflective light to reduce symptoms of eye strain.
If you think computer vision syndrome is affecting your eyes, please give us a call and we’ll be happy to set up an appointment to discuss your case.
By Dr. Nicholas R. Rader
Glaucoma is the second leading cause of blindness worldwide, behind cataracts. It is sometimes called the “silent thief” of vision because in its most common form — the one that affects 90% of glaucoma patients — there may be no symptoms until very late in the disease.
By that time, damage can be severe and irreversible. This is why regular eye exams are so important to detecting the disease in its earliest stages.
Although eye drops have been the mainstay of glaucoma treatment for many years, since the late 1960s the surgical procedure of choice has been trabeculectomy. With trabeculectomy, a surgical drain (fistula) is created so fluid can drain from inside the eye to a blister, or bleb, created on the surface of the eye.
Although you can greatly reduce pressure with trabeculectomy, there are many complications associated with this surgery. These include discomfort from the bleb, cosmetically unacceptable appearance of the eye, late infection that could lead to blindness, leakage of the bleb, failure of the bleb and the not-infrequent need for additional surgery.
Add to this the need for frequent follow-up visits and lifestyle limitations — many surgeons advise their patients against swimming and other physical activities after trabeculectomy — and it’s little wonder that surgeons have sought better, less invasive alternatives.
These newer procedures are designed to take advantage of the eye’s natural drainage mechanism. They are usually referred to as minimally invasive glaucoma surgery or MIGS.
Canaloplasty is one such procedure that has changed my own approach to glaucoma surgery. I performed my first canaloplasty shortly after the procedure was approved by the FDA in June of 2008, and it quickly became my preferred procedure for many reasons.
Rather than create a hole in the eye to relieve pressure, canaloplasty uses a small, 200 micron fiber optic catheter to re-open the normal outflow channels of the eye. It’s very similar to the way angioplasty opens the blocked vessels of the heart.
Since this does not involve creating a fistula to allow fluid to exit the eye, it eliminates the risks of infection, wound leakage and excessively low pressure associated with trabeculectomy. By expanding the eye’s existing drainage mechanism, canaloplasty controls the eye’s intraocular pressure in a physiologic manner.
Recovery is faster, fewer office visits are needed and costs are reduced. Best of all, the patient can more quickly resume normal activity.
Spawned by the success of the canaloplasty procedure, efforts are now underway to develop new procedures designed to take advantage of the internal drainage system of the eye.
Trabeculotomy, for instance, is a delicate electro-surgical procedure that has been available in the United States since 2006. It uses discrete electrocautery to open the internal access to the eye’s drainage system. I have found this to be useful in patients requiring mild reductions in pressure. Like canaloplasty, trabeculotomy can be performed in conjunction with standard cataract surgery.
In June 2012, the iStent was approved for use in the United States. At the time, it was the smallest device ever approved by the FDA. With this procedure, a microscopic drain is inserted to provide internal access to the eye’s existing drainage system. The results seem to be similar to those obtained with trabeculotomy, but continued modifications of the device may result in even better pressure control.
These are exciting times for eye surgeons. As we combine better understanding of the mechanisms behind glaucoma with creative developments in surgical equipment, we are able to fight the disease using the eye’s natural pressure control mechanisms.
I believe we can look forward to improved surgical outcomes for glaucoma with reduced risk of complication and less interference with our patients’ active lifestyles.
By Dr. Charles McCormick III
Assuming you haven’t been asleep at the wheel of life, you may have noticed lots of recent changes in the way health care is delivered in America.
Obviously this is a concern to many families. Today I’d like to give you a “peek behind the curtain” at the regulatory and administrative challenges from the perspective of a practicing physician.
Consolidation of physician practices into larger groups has been a major theme for the last 25 years. “Larger than ever” is the common tactic for survival. By grouping together, doctors can share expenses for administration and medical equipment, such as diagnostic machines that can cost $40,000 to $65,0000 each.
Here at the Indiana Eye Clinic, we strive to be a practice on the leading edge of technology, offering high-end eye care such as corneal mapping, laser-assisted cataract surgery and in vivo optical analysis. We are able to offer these treatments to our patients because we have built up a substantial practice over nearly 30 years.
Now imagine you are a young ophthalmic physician entering the workforce, usually with a mountain of student loan debt and little access to capital. Each of these pieces of high-cost gear represents a barrier to being able to perform quality work.
Group practices share an economy of scale with pooled computer systems, human resource manpower, rent and other expenses. As a result, smaller patient populations are underserved partly due to the poor capacity of smaller offices to amortize these costs.
Recently hospitals have been hiring physicians to serve in accountable care organizations (ACO). Having this third-party intrusion can further diminish a doctor’s capacity to ensure quality of care. The early data reports on rolling the doctor-patient relationship into a hospital ACO are not convincing.
Moreover, ACO physician satisfaction and compensation declines endanger sustainable working arrangements. Multi-specialty groups are likely to embrace similar strategies in hiring doctors, and unless they stay focused in promoting physician efforts for quality care, they will face similar challenges.
In this further build-out of health care groups, patients risk losing the personal attention they feel they deserve from the doctor entrusted with their care.
Many observers argue that healthcare is the most overregulated industry in the country. Medicare, Medicaid and the private insurance industry act as conduits for payment to hospitals, physicians, patients and pharmacists. Each channel is impacted by thousands of regulations, often with inadequate oversight, and subject to reimbursement fraud. The system is too complicated!
The Centers for Medicare and Medicaid Services (CMS) have sought to replace the International Classification of Diseases, ICD-9, with a new expanded ICD-10 that would increase the classification of all types of medicine from 28,000 codes to 260,000 codes. This is likely to further escalate unnecessary administrative expenses, but not enhance patient care.
CMS has already instituted physician quality reporting mandates that require electronic medical records, additional personnel and more technology. These added expenses are to be paid by physicians despite reduced reimbursements. So far in 2015, only 27% of practicing physicians have complied with the requested changes.
For Medicare, CMS has advised physician fee cuts of 2% to 20% this year – a nightmare that Congress may cancel with pending legislation known as the “doc fix.”
Further reductions in reimbursement will further constrain doctors’ capacity to comply or willingness to play along with onerous regulation. A significant number of Baby Boom physicians are choosing to retire instead of complying. In the eye care segment, we now have 11% fewer doctors serving a population that has grown by 11%!
The Affordable Care Act, commonly referred to as Obamacare, is a centrally administered plan that is neither affordable nor effective in addressing patient care needs, in my opinion. With ACA costs so absurdly out of order, many unintended consequences are in the offing. We may see more physician practices opting for a strict fee-for-service model, bypassing all third-party reimbursements like Medicare and private health insurance.
Finally, there is the issue of medical malpractice. Indiana has experienced less volatility in litigation than other states, due to a cap on emotional pain and suffering payments plus a physician panel review system established in 1975. Nonetheless, doctors are conditioned to regard a malpractice lawsuit as a “when,” not an “if.”
States with high rates for med-mal insurance essentially limit the service or deny access to it. Front-page jury awards, lifelong calculated disability and emotional pain risk are factored into insuring physician behavior.
Doctors and associated practitioners have much to be proud of in modern medical practices. However, the recent wave upon wave of regulations impacting the industry reflects our government’s attempt to address problems from Washington D.C. It will leave unintended potholes through which we all must navigate.
By Dr. David F. Box, Ophthalmologist
Macular Degeneration is a common diagnosis for patients over age 50. The incidence increases in each subsequent decade of life. Patients who receive this diagnosis often become emotionally distraught because they believe it always results in blindness.
While it is true that some cases can lead to central loss of vision, that is not true the majority of the time. Although there is still much to be learned about this ocular disease, active research is making progress and the overall prognosis is improving.
New medications have been developed and risk factors are being identified. There are several promising new treatments on the horizon that should improve the prognosis even more. The information for this article was obtained from the National Eye Institute.
The disease causes damage to the macula, which is a small area located in the central portion of the retina. The macula contains a high density of the visual nerves needed for sharp central vision. Patients with damage in the macular region of the eye will notice blurring and distortion of central vision. Sometimes this damage can be spotty and not all areas of the macula are equally involved.
In more severe cases, all of the macular cells are damaged and the patient will completely lose central vision in the affected eye. A person with loss of macular function would still have peripheral visual input but would lose ability to read, drive and recognize faces. Most of the cases involve both eyes, but the degree of severity between the two can vary significantly.
Another variable among patients is the rate of progression. The disease does not spontaneously improve and usually worsens gradually. Some patients have much faster progression than others. The rate of progression can also differ between eyes in the same patient.
There have been risk factors identified in macular degeneration patients. In general, age seems to be the most important risk factor. Often you will see the disease identified by the acronym AMD, which is an abbreviation for Age-Related Macular Degeneration.
Researchers are trying to learn more about the specific age changes occurring in the retinas of affected patients. Smoking has been shown to double the risk of AMD. People with a family history of AMD are also at a higher risk. AMD is more common among Caucasians than among African-Americans or Hispanics/Latinos.
Researchers have found links between AMD and some lifestyle choices. Patients may be able to reduce their risk of AMD or slow its progression by making these choices: avoid smoking, exercise regularly, maintain normal blood pressure and cholesterol levels, eat a healthy diet rich in green leafy vegetables and fish.
AMD can only be detected by a comprehensive dilated eye exam performed by an eye care professional. As in many medical conditions, an accurate and early diagnosis of AMD is important in developing a proper treatment plan and providing appropriate counseling to the patient tailored to their specific findings.
Unfortunately, AMD shares symptoms with many other eye conditions. Misdiagnoses can occur. A delay in the proper diagnosis could have a significant impact on the course of the disease. If a patient receives an improper diagnosis of AMD, then this can lead to avoidable anguish and fear for the patient and their family.
It is very important to make the proper diagnosis as early as possible in the course of AMD. Proper grading and staging of the severity of the disease in each eye is valuable for many reasons. In order to accomplish this objective, eye care professionals must possess proper training and experience in managing AMD. They must also have access to additional diagnostic tests and equipment.
At the Indiana Eye Clinic, all of our eye physicians are well-trained in the diagnosis and management of AMD. We also have the most advanced equipment currently available onsite to assist us in caring for our AMD patients.
In subsequent articles, I will discuss some more specific details about various types of AMD and current treatment options available.
By Dr. Michael L. Hopen, Ophthalmologist
Diabetes Mellitus, commonly referred to as simply diabetes, is a disease caused by excess blood sugar in the body over a period of time. Diabetes results from either the lack of insulin production or the body not responding normally to the insulin it does produce.
Diabetes is a condition that affects many tissues and organs in the body, including the eye. Some ways include:
Glasses prescription (refraction): Your prescription may be unstable if the blood sugar fluctuates too much. This will be perceived as blurry vision.
Lens: Diabetes can hasten the onset and progression of cataracts of the eye lens.
Optic Nerve: Diabetes can cause swelling and damage to the small blood vessels that nourish the optic nerve.
Retina: Diabetes can damage the small blood vessels that supply oxygen and nutrition to the retina. Over time, excess blood sugar can lead to small areas of bleeding, decreased blood flow and swelling of the retina.
If swelling affects the center part of the vision, this leads to “macular edema” which may require injections and/or a laser to treat. In more advanced stages, decreased blood flow can lead to the growth of new, more fragile blood vessels that are prone to bleeding. This could ultimately lead to irreversible vision loss.
Blood sugar and blood pressure control are the most important factors in preventing diabetic damage to the eye. Frequent dilated eye exams are essential to catching diabetic eye disease early in its course. The eye exams may need to be more frequent if the eye has already been affected.
Diabetes is a chronic condition that requires a great deal of attention from both patient and physician. At the Indiana Eye Clinic, your ophthalmologist or optometrist will keep in contact with your primary care physician (or endocrinologist) to communicate about factors results of the eye exam that are critical to the health of your eye and body.
Together, we can help protect your precious sense of sight from the worst effects of diabetes.